Heart attack is one of the most common reasons we BigD-ers shuffle off this mortal coil. Not because the kidneys have anything to do with managing our heart chemically, but because without kidneys we fill up with fluid and raise our blood pressure, putting stress on what is usually a pretty reliable ticker (heart failure is often the cause of death for people who decide not to go on, or give up dialysis). Constant fluid overloads over a long period gradually wear out hearts, they get tired and emotional and without regular maintenance, become unreliable, or worse.
My 19+years off and on dialysis (mostly on) makes me a paid-up member of this group. The main way my heart plays up is Atrial Fibrillation (AF), where it beats out of rhythm. AF can be anything from mild (I hardly notice it) to severe (where because it is doing such a lousy job of pumping blood and the oxygen it carries that I find it hard to stay upright). When in AF, my heart beats faster (to keep up the blood flow), but no matter how hard it tries, my blood pressure is always low. In fact, if I’m in the early stages, a fast pulse and low BP when I am clearly above my base weight are great indicators that I’ve gone into AF.
Of course there are side effects (besides being slower than a three-legged turtle). Because the heart is doing a lousy job of moving blood around, it can pool in inconvenient places, and even cause clots. Not good, but only disastrous if that happens in the brain (the most common cause of a stroke), or the heart (causing a heart attack). So if I’m in AF for more than a day or two, I take Warfarin, (Coumadin, Jantoven, Marevan, Uniwarfin) an anticoagulant, to minimise clotting. This in itself has an effect for BigD-ers: we must ensure that clinic staff know we’re on it so they can use a smaller amount of Heparin during each run, and I wait longer for bleeding to stop after the needles come out. This also applies to any cuts and scratches I inflict upon my body parts.
So the ideal situation is to not go into AF, or to catch it early.
Stopping it before it starts
The best way to stop it before it starts is to visit a cardiologist regularly. The cardiologist I go to is excellent. His stated aim is to keep people alive longer than we would be without his help – an excellent objective say I. And he’s done a sterling job so far. I’ve had AF for more than 10 years.
In the early days he zapped my heart back into rhythm with those electric paddles we have all seen on our favourite TV show (anyone remember Dr Ben Casey? Sadly I do… but I digress).
Since those early days, he has had me taking two heart medications:
- Metoprolol, a beta blocker (it blocks the electrical impulses that pass to the lower heart), that reduces heart rate and AF, and the force of heart muscle contractions to lower blood pressure. Since starting, I usually score a heart rate of around 55 BPM – much the same as all the athletic types in the family. Since I choose not to share how I achieve it, most people think I am incredibly fit, which I see this as a positive side effect
- Flecainide (Tambocor), which also blocks electrical signals in the heart that cause an irregular heartbeat, is used for serious AF (I used to take Amiodarone, but it gradually became less effective, so I was weaned off it and onto it’s big shot replacement).
These two have mostly kept AF at bay. Once in a blue moon I forget to take a dose, and AF can make a tentative appearance. But once these little white friends are back into my system, it fades away.
Catching it early
This was a little more difficult until recently. Apart from feeling “out of rhythm” and confirming it by checking my pulse (easy with a fistula), my main measure was the low BP/fast heart rate/above base weight I mentioned previously.
That was until I got my hands on a miracle machine. It came about like this. Julie went to see our No 2 son, Liam in London month or so ago. One of the social events he arranged was to get together with Malcolm, one of his excellent friends who stayed with us when he was a student doctor on placement at the Royal Melbourne Hospital. The world turned, as it is wont to do, and he is now Malcolm Finlay, Consulting Cardiologist (yes way!). He was trialling a new mini ECG/heart monitor for the iPhone, called the AliveCor Heart Monitor.

 Professional dialysis recruitment
Professional dialysis recruitment






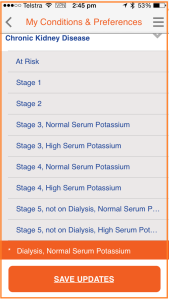
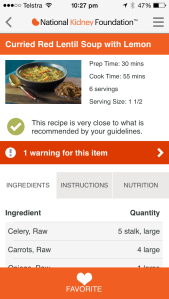
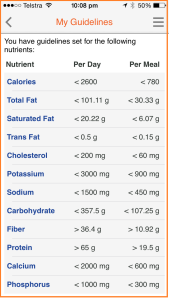 supermarket food item, recipe or a meal it measures it against the guidelines, and tells me if it is OK (with a green tick), is reasonably healthy, bad and or forbidden.
supermarket food item, recipe or a meal it measures it against the guidelines, and tells me if it is OK (with a green tick), is reasonably healthy, bad and or forbidden.